This blogpost is the final one of five looking at the Transforming
Care programme through the prism of the national statistics regularly produced
by the ever excellent @NHSDigital.
The first blogpost looked at the overall number of people
with learning disabilities and autistic people identified by the statistics as
being in inpatient services.
The second blogpost looked at statistics on the number of
people being admitted to inpatient services, and where they were being admitted
from.
The third blogpost looked at when people were in inpatient
units, how far were they from home and how long were they staying in inpatient
services.
The fourth blogpost looked at planning and reviews for
people within inpatient services.
This final blogpost will focus on the number of people
leaving inpatient services (charmingly called ‘discharge’ or 'transfer') and what is
happening leading up to people leaving. Again, even if the numbers of people leaving
are not yet rapidly changing as a result of Transforming Care, the impact of the
Transforming Care programme should be visible in the number of people getting ready to
leave and how well people’s plans to do so are developing.
The first and most obvious question is whether people in
inpatient services have a planned date to leave (I will pick up on the
complications of what ‘leaving’ actually means later in this post). The graph
below shows the proportion of people in inpatient services with a planned date
for transfer, from March 2015 to September 2016 (according to Assuring
Transformation data). There was a worrying drop in the proportion of people
with a transfer date in 2016, but by September 2017 over half of people (55%)
had a planned transfer date.
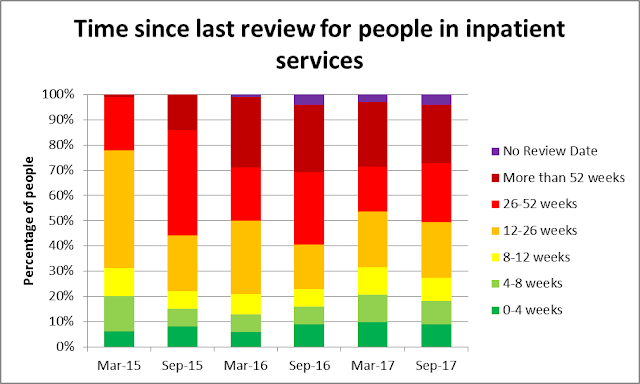
A date might be ‘planned’, but how distant in time is the
planned transfer? The 5 columns on the left of the graph below show this information
according to Assuring Transformation data, from March 2015 through to September
2017. Consistent with the earlier graph, the proportion of people without any
planned date to leave at all increased hugely in 2016, with the position
recovering throughout 2017. By September 2017, 11% of people had a planned
transfer date within the next 3 months, 16% had a planned transfer date between
3 and 6 months ahead, and 9% of people had a planned transfer date between 6
months and a year ahead. For 13% of people their planned date to leave was
between 1 and 5 years ahead, and for 7% of people their planned date to leave
was overdue.
The right hand column of the graph shows equivalent
information for August 2017 from the MHSDS dataset (see the first post in this
series for details of the two datasets), which focuses more on people with
learning disabilities and autistic people in more short-term mainstream mental
health services. Possibly because of the mainly short-term crisis nature of
people’s time in these services (in other words, people come in for a short period of time and leave again, with planned 'transfers' not part of the picture), the vast majority of people (87%) had no
planned date for transfer. The second post in this series showed that a large
proportion of ‘admissions’ to inpatient services were people transferred from
acute hospital services and readmissions (where people had previously been in an inpatient service less than a year before) – what’s happening to people in these
mainstream mental health inpatient services needs to be better understood.
So far, the statistics look like there is a push from
Transforming Care that is having an impact on the number of people with plans
to leave. Do we know anything about the plans themselves? Well, if people are
leaving the inpatient unit to go home in some sense then my expectation would
be that the person’s local council should be aware of the plan to leave. The
graph below shows information from Assuring Transformation based just on those
people with a plan to leave – for this group of people, are councils aware of
the plan? Over time, the proportion of people with a plan where their council
is aware of the plan is dropping – from over two thirds (69%) in March 2015 to
just over a half (53%) in September 2017. Just as worrying is that in September
2017, for a third of people (33%) it wasn’t known whether the council was aware
of the plan or not, a huge increase from March 2015 (7%). At the very least
this suggests that the close working between health and social care envisaged as
central to Transforming Care is not universally happening.
There are other signs too of potential haste in making plans
to leave. The Assuring Transformation statistics report whether a range of
people (the person themselves, a family member/carer, an advocate, the provider
clinical team, the local community support team, and the commissioners) have
agreed the plan to leave. For those people with a plan to leave, the graph
below reports the proportion of their plans that have been agreed by different people,
from March 2016 to September 2017. Over time, smaller proportions of plans have
been agreed by anyone and everyone potentially involved. By September 2017,
less than half of plans had been agreed by the person themselves (48%), a
family member (44%) or an advocate (48%). Only just over half of plans had been
agreed by the provider organisation (55%), the local community support team
(51%) or the commissioners (55%). Even though not everyone will be in contact with family members to agree these plans, for example, to what extent are these actually feasible
and sustainable plans that will result in a better life at home for people in
inpatient services?
The final graph in this short blogpost series is one of the
most important – how many people have actually been transferred from inpatient
services, and where have they gone? The graph below adds up monthly ‘discharges’
from inpatient services in the Assuring Transformation dataset for two periods
of time; a year from October 2015 to September 2016, and a year from October
2016 to September 2017. It’s also one of the most complicated graphs in this
series, so I’ll go through it in a bit of detail.
The first thing to say is that overall the number of people ‘transferred’
from inpatient services has increased, from 2,050 people in 2015/16 to 2,235
people in 2016/17.
Of the people who have been ‘discharged’, in 2016/17 almost
a quarter of people (525 people; 24%) moved to independent living or supported
housing. Another fifth of people (450 people; 20%) moved to their family home
with support, making nearly half of everyone ‘transferred’ from inpatient
services.
Where did everyone else go? For over a sixth of people in
2016/17 (375 people; 17%) their ‘discharge’ was actually a transfer to another
inpatient unit, confirming the picture of ‘churn’ of people passed around inpatient
services found elsewhere in this series. Even more people (410 people; 18%)
moved into residential care. Given that some inpatient services have re-registered themselves as residential care homes with the CQC, it is unclear
to what extent people are leaving an inpatient service to move somewhere more
local and homely, moving somewhere very similar to where they were, or not
actually moving at all but staying in a place that has re-registered.
In 2016/17, there were also another 195 people (9%) who
moved to an ‘other’ location – again it is unclear what these ‘other’ places
are, but are they wildly different from where people were moving from? Finally,
120 people (5%) are in the puzzling category of ‘no transfer currently planned’
while having apparently already been transferred.
So in this final post in the series, there are definite
signs that Transforming Care is exerting pressure for more people to have plans
to leave their current inpatient services, and almost half of those people who
are leaving are moving to independent or supported living or back to the family
home. There are also some worries about the feasibility and sustainability of
some of these plans, and the extent to which many people ‘leaving’ inpatient
services are actually leaving for something radically different or being
churned around a system that doesn’t call itself an inpatient service system but
looks mighty similar to the people living within it.
One final point - I started this short series of blogs with a warning from @MarkNeary1 that all these graphs and numbers are people - and then I spent five blogposts talking only about numbers. I hope that numbers (which is what I spend a lot of my working life trying to understand) can give part of the picture and are useful in encouraging change, but I do worry if I'm 'assuring' myself that this the case. I want to leave the final word to a tweet from @nbartzis which sums up the whole issue perfectly.
One final point - I started this short series of blogs with a warning from @MarkNeary1 that all these graphs and numbers are people - and then I spent five blogposts talking only about numbers. I hope that numbers (which is what I spend a lot of my working life trying to understand) can give part of the picture and are useful in encouraging change, but I do worry if I'm 'assuring' myself that this the case. I want to leave the final word to a tweet from @nbartzis which sums up the whole issue perfectly.